Innovative Care: Precision Medicine Empowered by Computer Vision

Table of Contents
- Introduction
- Need of Computer Vision
- Implementing a Model
- Challenges and Considerations
- Conclusion
- Frequently Asked Questions
Introduction
Meet Sarah, a 42-year-old mother of two who is battling breast cancer. It's a difficult period for her, filled with anxiety about what comes next.
Sarah has been informed she requires therapy, but the options are confusing.
She is only one of millions of women diagnosed with cancer each year. It's a terrifying statistic to be part of.
But Sarah is more than just a number; she is a person with her own life and body.
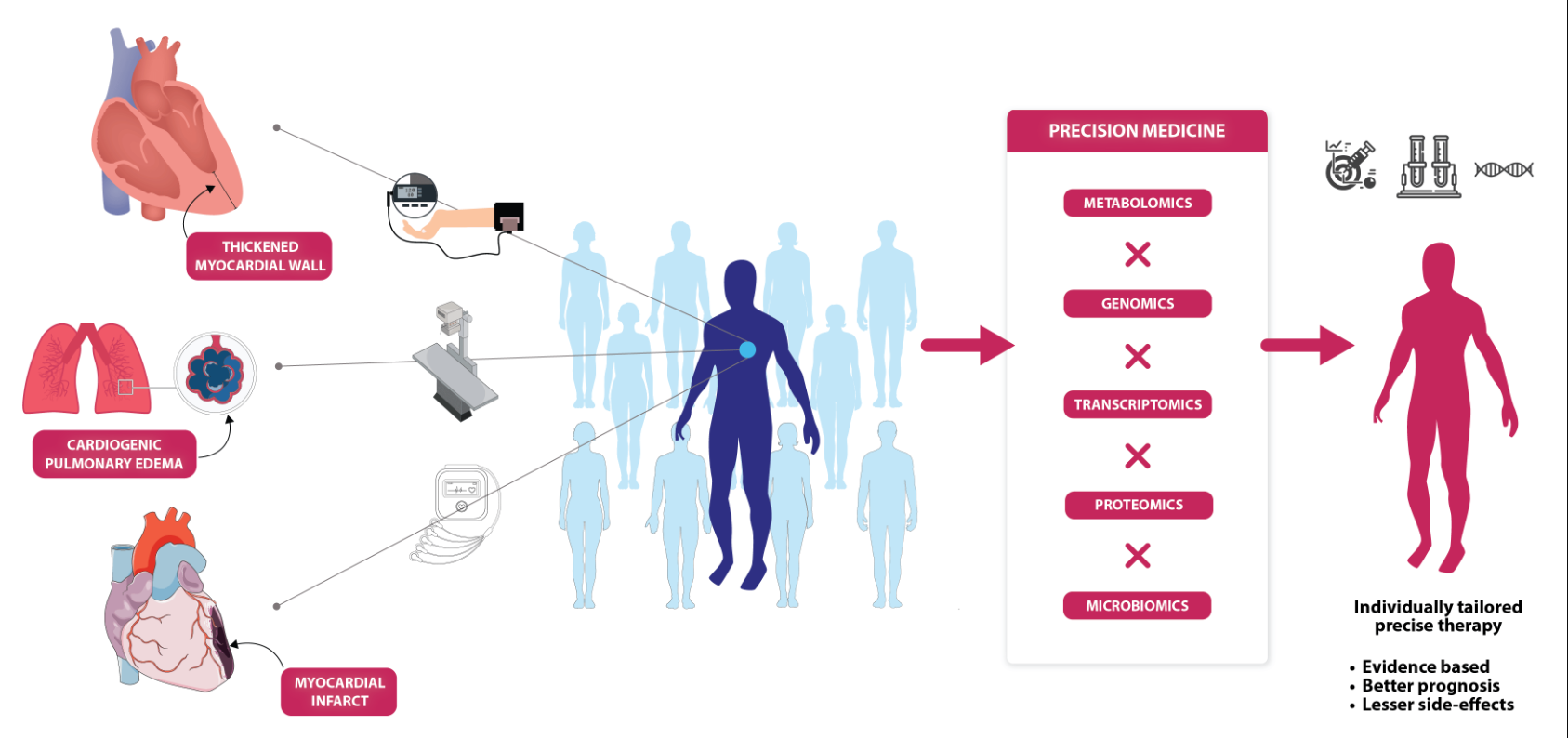
This is where precision medicine comes in. It is a revolutionary approach to healthcare that views each person as an individual rather than just another case.
For Sarah, this means that her physicians are closely monitoring her genes and cancer to determine the best treatment option. They are using all available information to devise a plan just for her.
Precision medicine is more than just a phrase; it's a true game changer.
With the worldwide precision medicine industry expected to increase from $29.1 billion in 2023 to $50.2 billion by 2028, more and more patients, including Sarah, will have access to personalised care.
Precision medicine is transforming the way we think about healthcare, making it more personalised and effective for everyone.
In this post, we'll look at how precision medicine and computer vision are improving healthcare.
Need of Computer Vision
Lets take a scenario of medical imaging, such as X-rays, MRIs, and CT scans, which plays a crucial role in diagnosing diseases and monitoring patient health.
However, the interpretation of these images can be time-consuming and subjective, leading to errors and delays in diagnosis and treatment.
This is where computer vision steps in, offering automated and objective analysis of medical images.
The incorporation of computer vision into precision medicine has huge potential and answers many important demands in healthcare.
Here's highlighting usecases of computer vision in the field of precision medicine:
1) Enhanced Medical Imaging Analysis:
- Medical imaging, such as X-rays, MRIs, and CT scans, is critical for illness diagnosis and therapy monitoring.
- Computer vision algorithms can analyse these photos with incredible speed and precision, allowing healthcare providers to detect irregularities, find patterns, and make more educated judgements.
2) Objective and Quantitative Analysis:
- Human interpretation of medical imaging is subjective and prone to inaccuracy.
- Computer vision offers an objective and quantitative method to picture processing, lowering variability and increasing consistency in diagnostic processes.
- This ensures that patients get precise and trustworthy assessments of their health conditions.
3) Early Disease Detection:
- Early detection of diseases improves patient outcomes by allowing for prompt interventions and therapies.
- Computer vision algorithms can detect small indicators of disease in medical photographs that humans may miss, allowing for earlier diagnosis and action and a better prognosis.
4) Personalised Treatment Planning:
- Precision medicine seeks to personalise medical treatments to individual patients based on their specific characteristics.
- Computer vision techniques can help identify biomarkers, genetic abnormalities, and other factors that affect illness development and therapy response.
- This data assists healthcare providers in designing personalised treatment regimens that maximise outcomes for each patient.
5) Efficient Workflow and Resource Allocation:
- By automating repetitive jobs and optimising workflow procedures, computer vision technologies can assist healthcare facilities in increasing efficiency and resource allocation.
- This allows healthcare providers to devote their time and expertise to tasks that require human judgement and intervention, hence improving patient care delivery.
6) Integration with Other Data Sources:
- In precision medicine, thorough patient profile requires data integration from a variety of sources, including clinical records, genetic data, and environmental factors.
- Computer vision algorithms may analyse and integrate data from multiple sources, offering a comprehensive picture of each patient's health status and allowing for more educated therapeutic decisions.
7) Research and Innovation:
- Computer vision helps to advance precision medicine research and innovation by allowing for large-scale analysis of medical imaging data, revealing new insights, and identifying novel biomarkers and targets for treatment.
- This promotes the creation of novel diagnostic instruments, helpful methods, and predictive models that enhance the field of precision medicine.
Implementing a Model
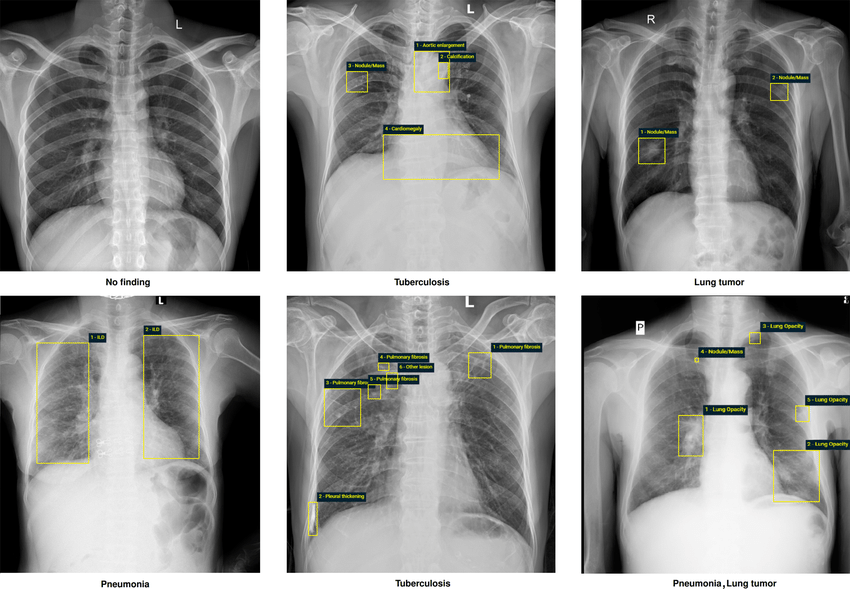
Let's consider a specific use case of implementing a computer vision model in radiology.
Imagine a scenario where radiologists need to analyze chest X-rays to detect and classify lung diseases, such as pneumonia, tuberculosis, and lung cancer.
Traditionally, radiologists manually review X-ray images, which can be time-intensive and prone to human error.
By developing a machine learning model trained on a dataset of annotated chest X-rays, we can automate the process of lung disease detection and classification.
The model learns to identify patterns and abnormalities indicative of different lung conditions, enabling rapid and accurate diagnosis.
This not only streamlines the workflow for radiologists but also ensures consistent and reliable results.
Now, let's develop a machine learning model for classifying lung diseases using chest X-ray images.
1. Data Gathering
- Collect a diverse dataset of chest X-ray images from reputable sources or healthcare institutions.
- Ensure that the dataset includes a sufficient number of images for each lung disease category of interest, such as pneumonia, tuberculosis, lung cancer, and normal (healthy) cases.
- Each image should be labeled with the corresponding lung disease category to facilitate supervised learning.
- Carefully label relevant features. Employ expert annotations or crowdsourcing for complex tasks(like Labellerr etc).
2. Data Preprocessing:
- Preprocess the chest X-ray images to standardize their size, resolution, and orientation.
- Convert the images to a consistent format (e.g., JPEG or PNG) and resize them to a uniform dimension suitable for input to the neural network model.
- Normalize the pixel values of the images to a range between 0 and 1 to improve model convergence during training.
3. Model Architecture:
- Design a convolutional neural network (CNN) architecture tailored for image classification tasks.
- A typical CNN architecture consists of alternating convolutional layers, activation functions (e.g., ReLU), pooling layers (e.g., max pooling), and fully connected layers.
- Experiment with different CNN architectures, including variations of popular architectures like VGG, ResNet, or DenseNet, to find the best-performing model for lung disease classification.
4. Data Augmentation:
- Augment the training dataset using techniques like rotation, scaling, flipping, and shifting to increase dataset diversity and improve the model's generalization ability.
- Data augmentation helps prevent overfitting and enables the model to learn robust features from a limited amount of training data.
5. Model Training:
- Split the preprocessed dataset into training, validation, and test sets. Typically, the dataset is partitioned into a training set (e.g., 70-80% of the data), a validation set (e.g., 10-15% of the data), and a test set (e.g., 10-15% of the data) for model evaluation.
- Train the CNN model using the training dataset and validate its performance using the validation dataset.
- Use optimization techniques such as stochastic gradient descent (SGD), Adam, or RMSprop to update the model parameters iteratively and minimize the classification error (loss function).
6. Model Evaluation:
- Evaluate the trained CNN model's performance using the test dataset, which contains unseen examples not used during training or validation.
- Calculate evaluation metrics such as accuracy, precision, recall, and F1-score to assess the model's classification performance across different lung disease categories.
- Visualize the model's predictions and confusion matrix to gain insights into its strengths and weaknesses in classifying lung diseases from chest X-ray images.
7. Model Deployment:
- Deploy the trained CNN model in a real-world healthcare setting, ensuring compliance with regulatory standards and data privacy requirements (e.g., HIPAA compliance).
- Develop a user-friendly interface or integrate the model into existing healthcare systems to enable healthcare professionals to upload chest X-ray images and receive automated predictions of lung disease categories.
- Continuously monitor and evaluate the model's performance in the production environment, and update the model periodically to adapt to evolving clinical requirements and data distributions.
- By following these comprehensive steps, healthcare professionals and data scientists can develop a robust machine learning model for lung disease classification using chest X-ray images, thereby aiding in the diagnosis and treatment of patients with respiratory conditions.
By following these steps, we can build a robust machine learning model for lung disease classification that can assist healthcare professionals in diagnosing and treating patients more effectively.
Challenges and Considerations
While computer vision holds immense promise in healthcare, it also presents several challenges that need to be addressed:
- Data Quality and Quantity: The performance of computer vision models heavily relies on the quality and quantity of annotated medical imaging data. Acquiring large and diverse datasets that accurately represent different disease conditions can be challenging.
- Interpretability and Trust: Understanding how computer vision models arrive at their decisions is crucial for building trust among healthcare professionals. Interpretable machine learning techniques and model explainability tools are essential for ensuring transparency and accountability.
- Regulatory Compliance and Ethics: Deploying computer vision systems in healthcare requires adherence to strict regulatory standards, such as patient privacy regulations (e.g., HIPAA) and ethical considerations regarding data usage and patient consent.
- Integration with Clinical Workflows: Seamless integration of computer vision technology into existing clinical workflows is essential for maximizing its impact and adoption. User-friendly interfaces and interoperability with electronic health record systems are key factors to consider.
Conclusion
In conclusion, computer vision has the potential to revolutionize healthcare by augmenting medical imaging analysis, diagnosis, and treatment planning.
By harnessing the power of advanced algorithms and machine learning, healthcare providers can leverage automated image interpretation to improve patient outcomes and streamline clinical workflows.
However, reaching the full potential of computer vision in healthcare requires coordination among healthcare experts, data scientists, regulators, and technology developers.
Together, we can overcome challenges, address ethical concerns, and harness the transformative capabilities of computer vision to build a healthier and more equitable future for all.
Frequently Asked Questions
Q1.What technologies are used in precision medicine?
Precision medicine uses biological signs called biomarkers to precisely characterise a patient's genotype, or genetic code, and phenotype, or physical attributes, as well as to classify patients based on their response to treatment and/or risk for specific diseases.
Q2.How is artificial intelligence used in precision medicine?
Through the use of precision medicine techniques, patient phenotypes with uncommon therapeutic responses or distinct medical requirements are identified. Artificial intelligence (AI) uses complex calculation and inference to produce insights, gives the system the ability to reason and learn, and enhances human decision-making in clinicians.
Simplify Your Data Annotation Workflow With Proven Strategies
.png)