Insurance Fraud Detection using NLP: How It Works

Table of Contents
- Introduction
- Role of NLP in Fraud Detection
- Real Life Scenario
- How Do NLP Powered Companies Detect Insurance Fraud?
- Companies That Offer Insurance Fraud Detection Solutions Powered by NLP
- How Can Labellerr Help Create Training Data for NLP Model?
- Types of Insurance Fraud
- Benefits of NLP in Insurance Fraud Detection
- Challenges
- Conclusion
- Frequently Asked Questions
Introduction
For insurance industry, fraud poses a significant threat to both insurers and policyholders, which results in immense financial losses and compromised trust within the industry.
Life insurance fraud represents one of the most costly challenges in the insurance industry. Common life insurance fraud includes staged deaths, falsified medical records, and beneficiary fraud..
Modern insurers need advanced solutions to combat these evolving threats. This is where NLP-powered fraud detection becomes essential for life insurance companies.
Insurance fraud is a significant concern, costing the industry billions of dollars annually.
Insurance fraud is estimated to cost insurers billions of dollars annually worldwide, exerting immense strain on industry profitability.
This criminal activity not only impacts insurers financially but also drives up premiums for honest customers, making everyone a victim.
Insurance fraud includes various deceptive practices aimed at exploiting insurance policies for financial gain. These fraudulent activities can occur in multiple forms, including falsifying claims, staging accidents, or providing misleading information during the application process.
Identifying and mitigating such fraudulent behaviors is paramount for insurers to maintain their financial stability and uphold the integrity of their services.
Role of NLP in Fraud Detection
Natural Language Processing, a branch of artificial intelligence, equips insurers with the ability to analyze and interpret vast amounts of textual data present in insurance claims, policy documents, and customer communications.
By leveraging NLP techniques, insurers can uncover patterns, anomalies, and indicators of potential fraud that may avoid traditional detection methods.
In insurance, NLP techniques are utilized to analyze vast amounts of unstructured text data, such as claims forms, policy documents, correspondence, and notes, to uncover patterns, anomalies, and inconsistencies indicative of fraudulent behavior.
One key aspect of NLP in fraud detection is the ability to extract relevant information from text through techniques like named entity recognition, sentiment analysis, and semantic analysis.
NLP models can automatically identify entities, such as names, dates, locations, and monetary amounts, which allows them to flag suspicious entities or relationships that may signify fraudulent activities, such as inflated claims or falsified information.
NLP increases efficiency by automating analysis, saving time and resources compared to manual review.
Additionally, NLP can enable the early detection of fraud, potentially leading to the prevention of significant losses for insurance companies and their policyholders.
Let’s understand insurance fraud with the help of an example:
Real Life Scenario
John submits an insurance claim stating that his car was involved in a collision with another vehicle at an intersection on January 15th, 2024, at 3:00 PM.
He provides a detailed description of the accident, claiming that the other driver ran a red light, causing the collision.
John states that the weather was clear, and the road conditions were dry at the time of the accident. He also submits photographs of the damage to his vehicle as evidence.
How NLP Would Detect the Fake Claim:
Named Entity Recognition (NER):
- NLP algorithms identify and extract entities such as dates, times, locations, and vehicle descriptions mentioned in the claim.
- In this case, NER would extract entities like "January 15th, 2024", "3:00 PM", "intersection," and potentially the make and model of the vehicles involved.
Semantic Analysis:
- Sentiment Analysis: NLP algorithms analyze the sentiment expressed in the claim description. If John's language appears overly dramatic or exaggerated, it could indicate potential deception.
- Entity Relationships: NLP models examine the relationships between the entities mentioned in the claim. For example, inconsistencies between the claimed location of the accident and known accident data for that intersection could raise suspicion.
Topic Modeling:
- NLP techniques like Latent Dirichlet Allocation (LDA) could identify common topics or themes within the claim description. Any inconsistencies from typical accident narratives could be flagged as potential fraud indicators.
Contextual Analysis:
- NLP models utilize contextual embeddings like BERT to understand the context of the claim description. They can capture complex linguistic signs or inconsistencies that might suggest deception.
Integration with Fraud Detection Systems:
- NLP insights are integrated into a larger fraud detection system that combines NLP analysis with other data sources such as accident reports, traffic camera footage, and historical claim data. Any discrepancies between John's claim and the available data would be investigated further.
Continuous Learning:
- The NLP model is continuously updated and trained on new data to adapt to evolving fraud tactics. Feedback from identified fraudulent claims is used to improve the model's accuracy over time.
In this scenario, NLP techniques would help insurance investigators identify inconsistencies or red flags in John's claim, such as discrepancies in the claimed location, time, or weather conditions.
By leveraging NLP alongside other fraud detection methods, the insurance company can prevent fraudulent payouts and protect against financial losses.
Labellerr's annotated training data enables such precise detection. Our annotations help NLP models recognize subtle fraud patterns.
How do NLP powered companies detect insurance fraud?
NLP-based fraud detection companies use scales and ratings to classify potential claim fraud. Here's a breakdown of how this process generally works:
1. Fraud Indicators and Scoring:
- NLP (Natural Language Processing) is used to analyze textual data within claims, such as adjuster notes, medical reports, or witness statements. It identifies keywords, phrases, inconsistencies, and patterns that may suggest fraudulent activity.
- The platform examines patterns of behavior in claims data and compares them to known fraudulent tactics. This includes things like frequent changes of address, multiple claims within short periods, or inconsistencies in descriptions of incidents.
2. Fraud Suspicion Score:
Each claim is assigned a fraud suspicion score based on the presence and strength of the indicators identified. This score is usually numeric and indicates the likelihood of the claim being fraudulent.
3. Classification and Thresholds:
Insurers set thresholds for fraud suspicion scores. Claims exceeding the threshold are flagged for further investigation by an SIU (Special Investigations Unit). Companies use terms like:
- High Suspicion: Strong indicators of fraud warrant a deeper investigation.
- Moderate Suspicion: Potential red flags requiring additional scrutiny.
- Low suspicion: minimal indicators, less likely to be fraudulent.
4. Prioritization and Investigation:
Claims with high suspicion scores are prioritized for investigation .Investigators leverage the insights from the fraud detection platform alongside their own expertise, additional evidence gathering, and analytical methods to confirm or deny fraudulent intent.
Companies that offer insurance fraud detection solutions powered by NLP
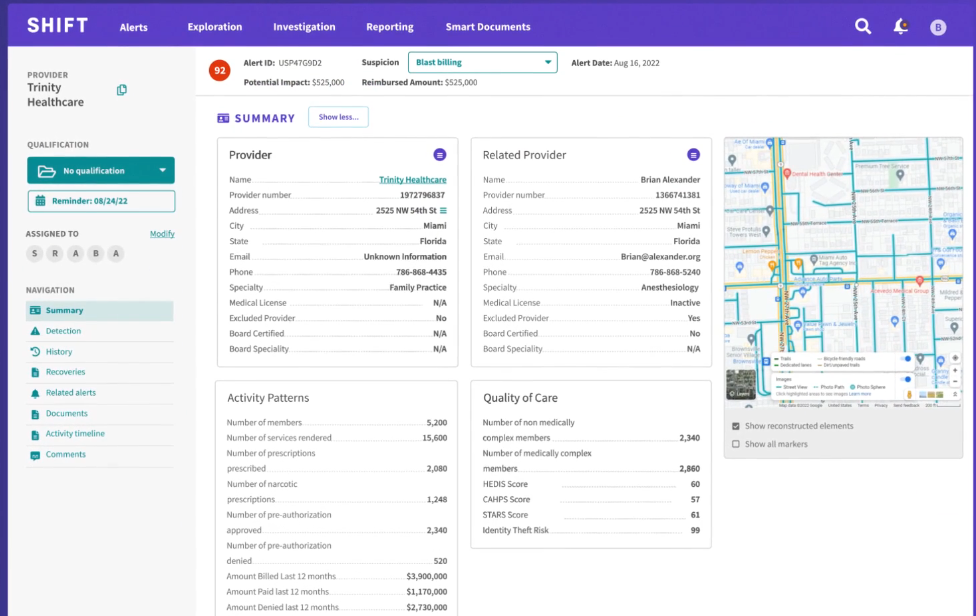
- Advanced Machine Learning Algorithms:
The platform uses machine learning algorithms to analyze vast amounts of data and detect patterns indicative of fraudulent activities. These algorithms continuously learn and adapt to new fraud tactics, enhancing the accuracy of detection over time.
2. Real-Time Monitoring:
Shift Technologies' platform provides real-time monitoring of transactions and user activities, allowing for immediate detection and response to suspicious behavior. This capability minimizes the risk of fraudulent transactions slipping through unnoticed.
3. Customizable Rules Engine:
Users have the flexibility to create and customize rules tailored to their specific business needs and risk thresholds. This customizable rules engine ensures that the platform can adapt to different industries and evolving fraud trends effectively.
2) FRISS:
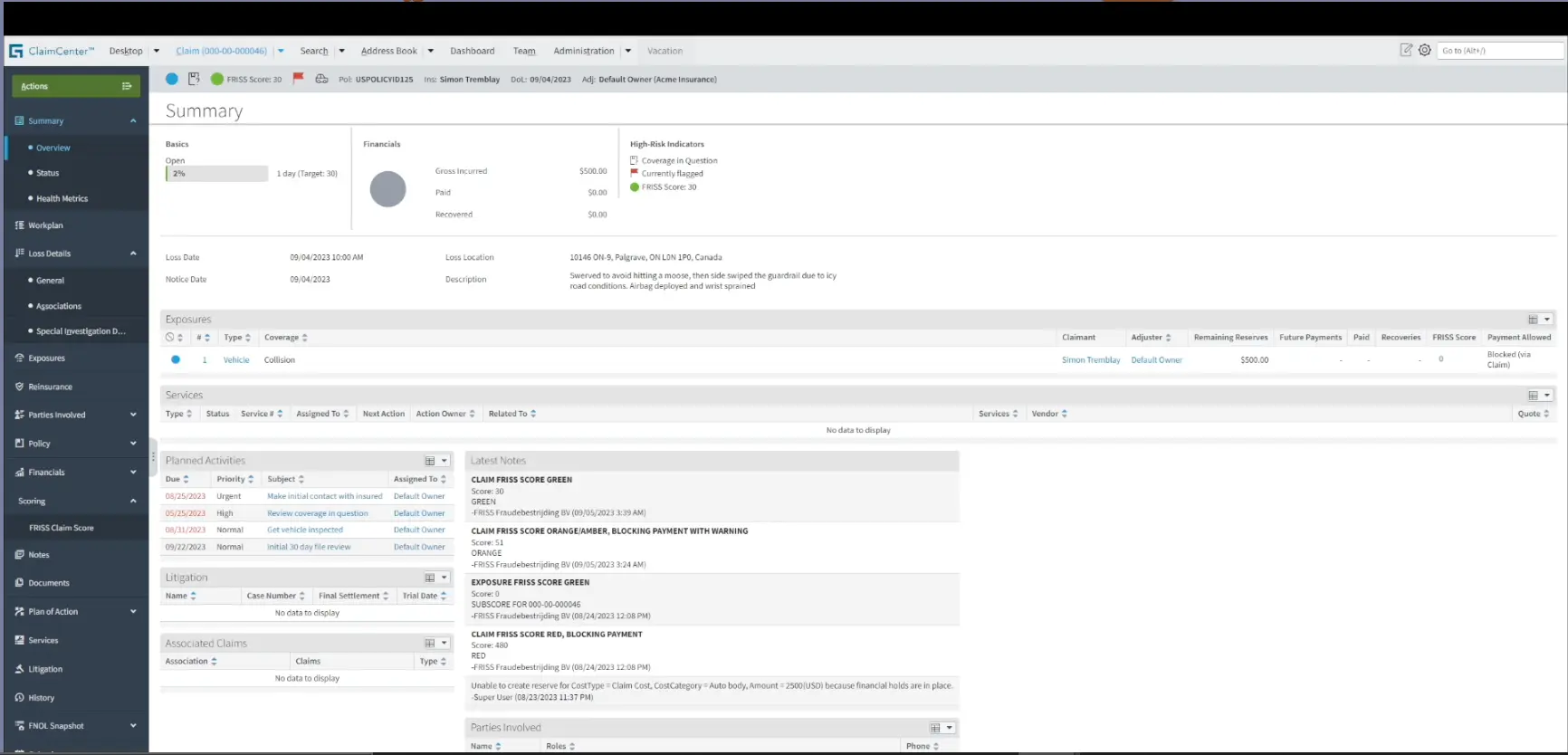
1. Data Consistency
Data consistency is key. Integrating your case management tool with your core systems ensures data consistency and accuracy.
When information is automatically synchronized across different platforms, you can trust that the data is up-to-date and reliable. Don’t get lost in a version control spiral.
2. Streamline Workflow
Case management integration enables automated workflows and streamlined processes. For example, if your case management tool is integrated with your core system, you can automatically create new cases or update customer records based on specific triggers or events.
3. Enhanced Collaboration
Integration of a core system and case management software fosters collaboration among different teams or departments within your organization.
Relevant information from various systems can be shared seamlessly, allowing investigators, case managers, legal teams, and other stakeholders to access and collaborate on case-related data in real-time.
4. Real-time Reports
By integrating case management tools with the organization's core systems, organizations can leverage the combined data to generate comprehensive reports and perform in-depth analysis.
This view provides valuable insights into trends, patterns, and performance metrics across different aspects of your organization.
3) SAS Fraud and Security Intelligence:
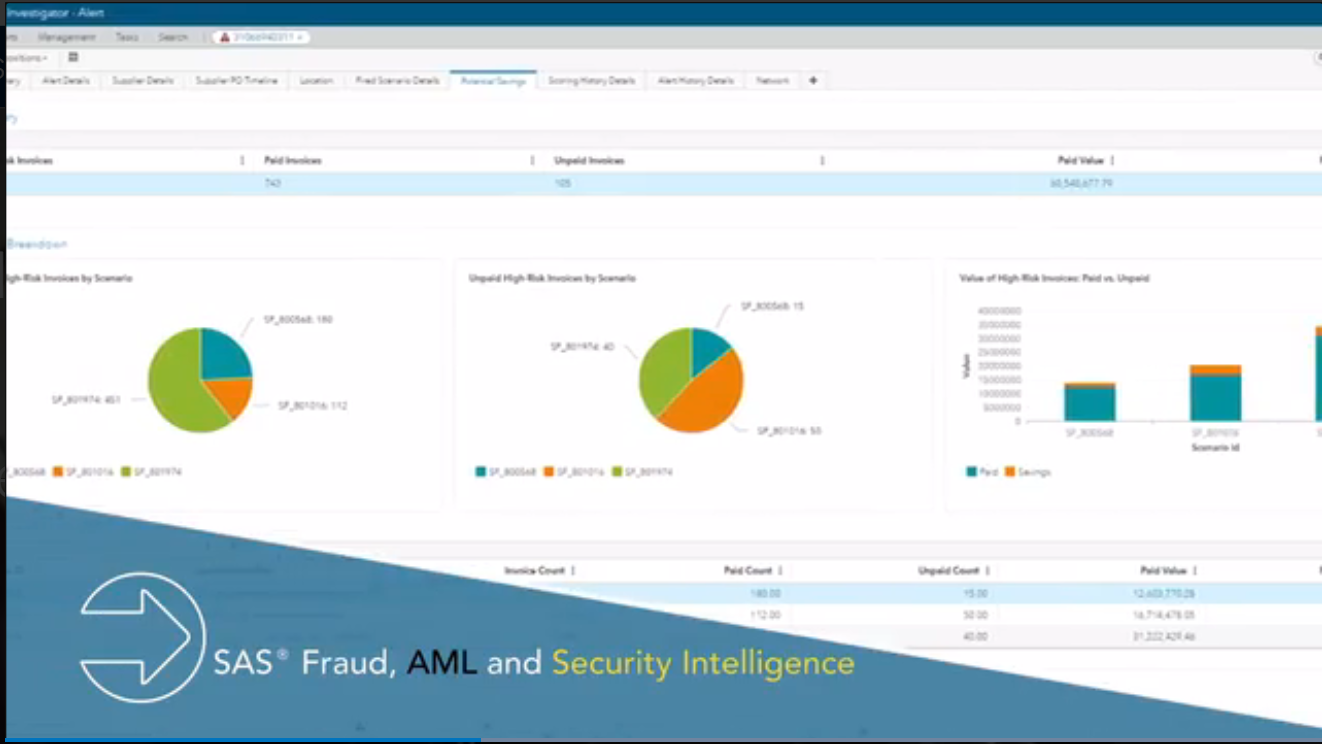
1) Real-time scoring & decisioning
SAS can score and make decisions on 100 percent of all transactions (purchase, payments, and nonmonetary events) on demand in real-time, as well as in near-real-time or batch modes.
Handle any data in real time with the industry's highest throughput (>10,000 transactions per second) and lowest latency (<50 milliseconds).
2) Enterprise solution on a single platform
SAS allows a single installation of the software among independent departments with logical or physical multitenancy capability.
It can scale vertically or horizontally to support current and future infrastructure and business needs. It is highly secure and can integrate with an organization’s authentication services (LDAP, AD, etc.).
3) Simplified data management
SAS provides an external messaging API for easy integration with fulfillment decisions, external triage, case management and reporting systems.
It consists of a single interface for accessing the solution from multiple client-source systems or third-party data providers.
How can Labellerr help create training data for NLP model?
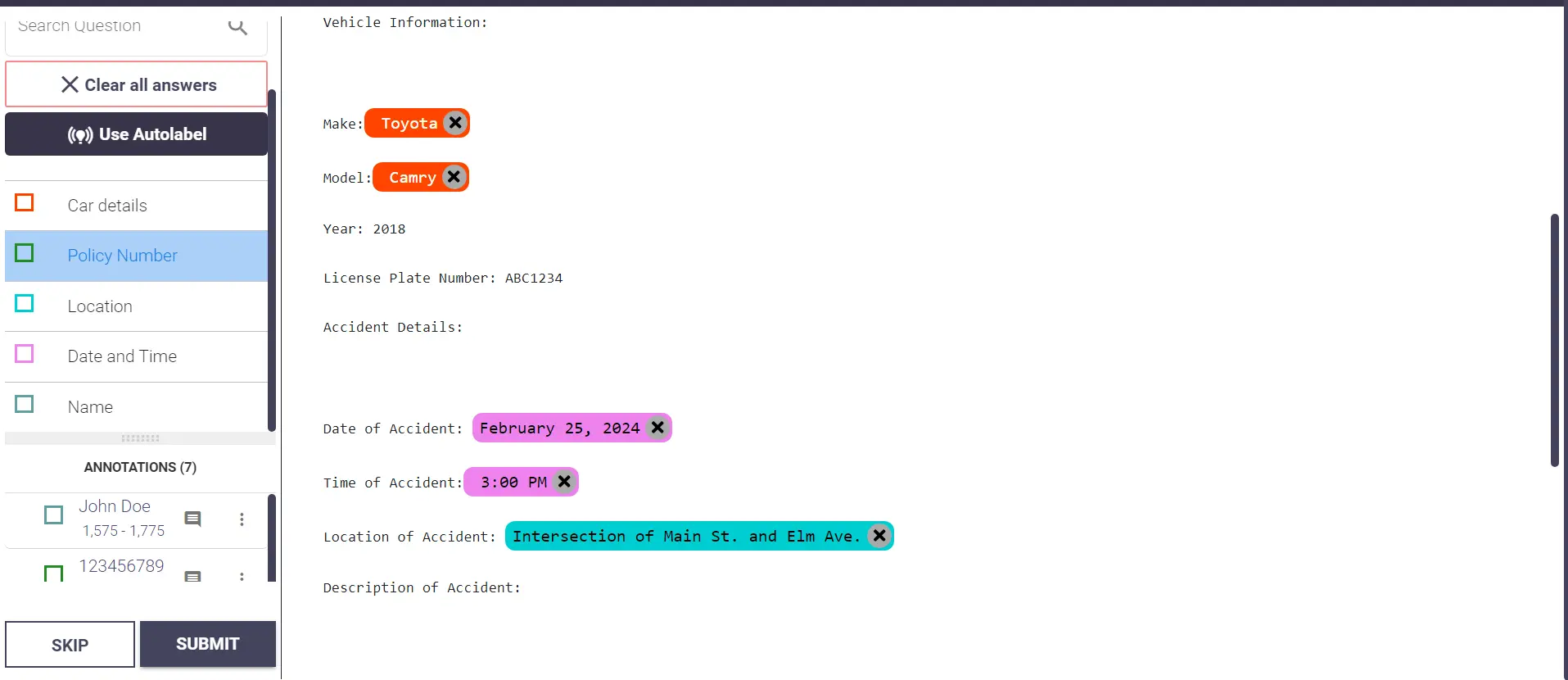
Labellerr can significantly help in text annotation for insurance fraud detection by providing a platform for efficiently labeling and annotating textual data with relevant fraud indicators.
With Labellerr, insurance companies can streamline the process of annotating large volumes of unstructured text data, such as claims forms, policy documents, and correspondence, by leveraging a combination of human annotators and machine learning models.
Firstly, Labellerr allows insurance professionals to define specific fraud indicators or patterns that they want to identify within the text data. These could include keywords or phrases indicative of fraudulent behavior, such as "exaggerated injury," or "falsified documentation,".
Secondly, Labellerr enables the annotation of text data by human annotators who are trained to recognize and label instances of fraud indicators within the documents. These annotations provide labeled datasets that serve as training data for NLP models, enhancing their ability to automatically identify fraudulent activities in future documents.
Types of Insurance Fraud
NLP can be applied to detect various types of insurance fraud across different insurance categories:
1. Auto Insurance:
NLP models can analyze narratives for inconsistencies, identifying unusual language patterns and comparing details with external data like police reports. It can detect inconsistencies in vehicle descriptions, ownership records and repair costs.
2. Property and Casualty Insurance:
NLP models can analyze narratives to identify any suspicious language patterns related to the cause and extent of damage, and comparing details with weather reports or imagery. It can also find any inconsistencies in descriptions of ownership records, and police reports.
3. Health and Life Insurance:
NLP models can find any differences in patient information, medical history and treatment details. It detects any fraudulent billing practices that provide claims for more expensive services than are actually delivered. It can also analyze death certificates, beneficiary information, and communication patterns for inconsistencies.
Labellerr's annotation platform helps train these specialized NLP models. Identify fraud patterns, creating high-quality training datasets. Train your model by detecting life insurance fraud more effectively with Labellerr's annotation solutions.
Benefits of NLP in Insurance Fraud Detection
- Enhanced Accuracy
The NLP algorithm can analyze textual data with very good accuracy, and fewer false positives and false negatives in fraud detection as compared to conventional methods.
2. Automated Claim and Prioritization
NLP-powered systems can automatically process incoming insurance claims based on their level of risk or suspicion. By analyzing claim descriptions and related documents, NLP models can assign priority levels to claims, ensuring that investigators focus their attention on high-risk cases first.
3. Cost Efficiency
By automating the fraud detection process, NLP helps insurers streamline operations, reduce manual effort, and allocate resources more efficiently, resulting in cost savings over time.
4. Automated Data Extraction
NLP algorithms can extract relevant information from unstructured data sources such as claim forms, policy documents, emails, and customer communications. Instead of manually reading through each document, NLP models can parse and extract key entities like names, dates, amounts, and descriptions, saving considerable time and effort.
5. Real-time Monitoring and Alerting
NLP-based systems can continuously monitor insurance data streams, such as claims submissions, policy updates, or customer communications, in real-time. By applying NLP techniques for text analysis and anomaly detection, these systems can identify potentially fraudulent activities and trigger automated alerts or notifications for further investigation, enabling proactive fraud prevention measures.
Challenges
NLP models rely heavily on the quality of training data. Inconsistent or incomplete information can lead to inaccurate fraud detection.
Insurance terminology and documentation are highly specialized, presenting challenges for generic NLP models trained on general-purpose use cases.
In insurance fraud detection, fraud claims represent only a small fraction of overall claims, resulting in imbalanced datasets where positive instances are significantly outnumbered by negative instances.
This highly imbalances the dataset and increases the bias. Another challenge is privacy and security.
Insurance data, which may contain sensitive personal information, and NLP-based fraud detection systems must adhere to strict data privacy and compliance standards, ensuring that sensitive information is handled and processed securely while maintaining regulatory compliance.
Our platform helps you annotate claims and documents to train powerful NLP models. Get started now
Conclusion
In conclusion, the application of Natural Language processing (NLP) in insurance fraud detection has emerged as a powerful weapon in this ongoing battle.
By analyzing large amounts of textual data, identifying inconsistencies, and extracting crucial information, NLP empowers insurers to detect fraudulent claims with greater accuracy and efficiency.
Furthermore, the potential of NLP extends beyond fraud detection. By gaining deeper insights into customer behavior and language patterns, NLP can contribute to improved risk assessment, personalized insurance products, and ultimately, a more customer-centric insurance experience.
Labellerr helps to build superior fraud detection systems through high-quality training data annotation. Our specialized approach to life insurance fraud detection ensures your NLP models achieve industry-leading accuracy. Contact us to train your Model
Frequently Asked Questions
1. What is insurance fraud, and why is it a significant concern for the insurance industry?
Insurance fraud involves the deliberate manipulation of insurance processes for financial gain. It poses a significant threat to insurers and policyholders due to its potential to incur substantial financial losses, increase premiums, and undermine trust in the insurance system.
2. How can Natural Language Processing (NLP) be used to detect insurance fraud?
NLP analyzes vast amounts of textual data related to claims, such as narratives, reports, and communication transcripts. It identifies inconsistencies, extracts key information, and gauges emotional tone to flag suspicious claims with a high probability of being fraudulent.
Simplify Your Data Annotation Workflow With Proven Strategies
.png)